Main Second Level Navigation
Mar 6, 2018
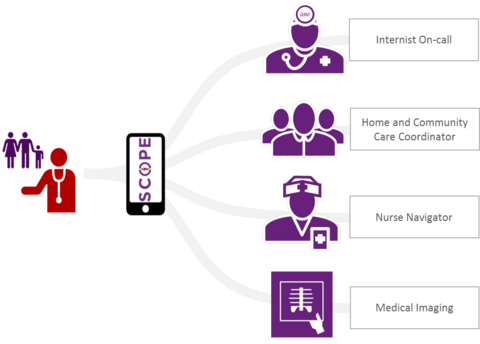
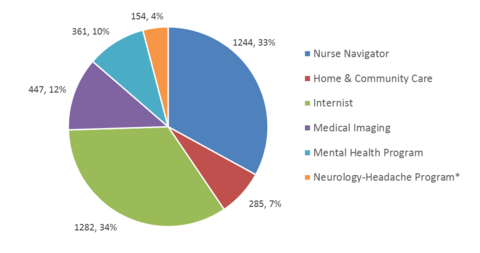
Chair's Column: Innovations in Primary-Specialty Care for Complex Medical Patients: The Value of Partnership
About Us, Cardiology, Clinical Immunology & Allergy, Clinical Pharmacology & Toxicology, Division of Dermatology, Education, Emergency Medicine, Endocrinology & Metabolism, Faculty, Gastroenterology & Hepatology, Geriatric Medicine, Hematology, Infectious Diseases, Medical Oncology, Nephrology, Neurology, Occupational Medicine, Palliative Medicine, Physical Medicine & Rehabilitation, Quality & Innovation, Research, Respirology, Rheumatology