Main Second Level Navigation
Nov 2, 2020
Pivoting to virtual care during the pandemic: How our CQIs responded
Cardiology, Clinical Immunology & Allergy, Clinical Pharmacology & Toxicology, Division of Dermatology, Education, Emergency Medicine, Endocrinology & Metabolism, Faculty, Gastroenterology & Hepatology, General Internal Medicine, Geriatric Medicine, Hematology, Infectious Diseases, Medical Oncology, Nephrology, Neurology, Occupational Medicine, Physical Medicine & Rehabilitation, Quality & Innovation, Respirology, Rheumatology, Palliative Medicine
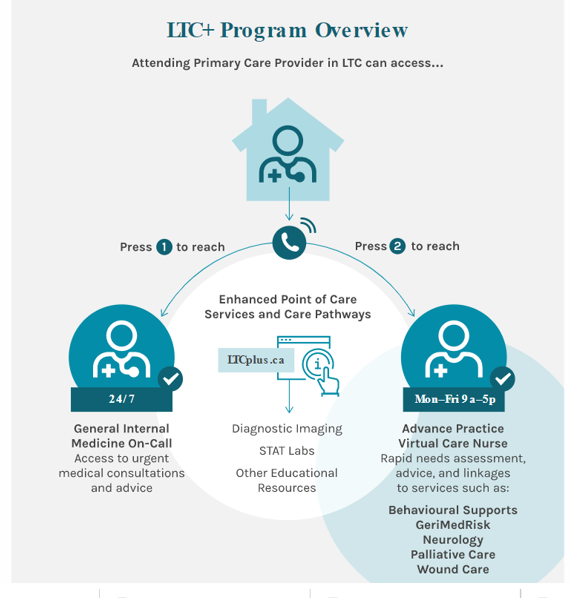

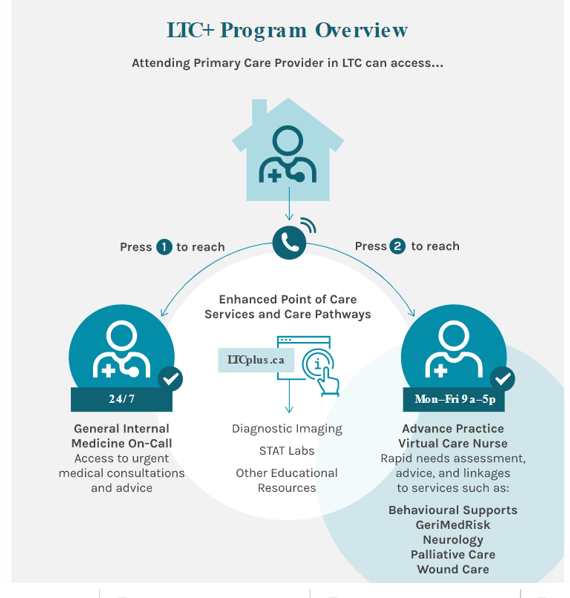 While many quality and innovation (QI) projects were halted as a result of the lockdown, many new projects were developed in relation to the pandemic, including LTC+. LTC+ is a hub and spoke model for providing virtual specialist care to residents of 52 long-term care centres (LTCs) in the Greater Toronto Area. Led by clinicians, researchers, and operational staff at Women’s College Hospital and WIHV, Sunnybrook, Unity Health, and Baycrest, this massive collaboration has integrated Toronto Paramedics services and community providers’ diagnostic imaging and laboratory tests into a care delivery model bar none.
While many quality and innovation (QI) projects were halted as a result of the lockdown, many new projects were developed in relation to the pandemic, including LTC+. LTC+ is a hub and spoke model for providing virtual specialist care to residents of 52 long-term care centres (LTCs) in the Greater Toronto Area. Led by clinicians, researchers, and operational staff at Women’s College Hospital and WIHV, Sunnybrook, Unity Health, and Baycrest, this massive collaboration has integrated Toronto Paramedics services and community providers’ diagnostic imaging and laboratory tests into a care delivery model bar none.
