Main Second Level Navigation
- Welcome
- Why Toronto?
- History of the Department
- Vision & Strategic Priorities
- Our Leadership
- Our Support Staff
- Location & Contact
- Departmental Committees
- Department of Medicine Prizes & Awards
- Department of Medicine Resident Awards
- Department of Medicine: Self-Study Report (2013 - 2018)
- Department of Medicine: Self-Study Report (2018 - 2023)
- Communication Resources
- News
- Events
Chair's Column: The Department’s Five-Year Review


On December 3 and 4, 2018 the Department of Medicine will be undergoing its five-year external review. Two reviewers have been selected by the Dean – Drs. Katrina Armstrong and Graydon Meneilly from Harvard Medical School and University of British Columbia, respectively – their profiles can be read here.
The Department’s Self-Study has been prepared by the Department leadership team made up of faculty and staff, with some help from the IM Chief Medical Residents. It builds on what we have learned from the 2015 and 2017 faculty surveys, resident and fellow feedback, external divisional reviews, and informal and formal feedback received every day. The full report is available online for your review: Volume 1 and Volume 2. Some of you have been invited to meet with the reviewers and others will have been asked to serve on the Dean’s Advisory Committee, which will ultimately make the recommendation on my reappointment as Chair of the Department of Medicine. Thank you in advance for your engagement and input!
Our mission is to prepare future physician leaders, contribute to our communities and improve the health and healthcare experiences of individuals and populations through the discovery, application, translation and communication of knowledge.
Our vision is to meaningfully impact health through international leadership in education, research and the translation of new knowledge into better care and health outcomes.
Fast Facts: DoM in 2018
- 789 full time and 652 part time and adjunct faculty members
- 36% clinician teachers & 48% clinician investigators or scientists
- 39% full time faculty are female (36% in 2013)
- 45% DoM leaders are female and 30% identify as visible minorities (26% and 10.5% in 2013)
- $185.448 million in research funding (2017)
- 23,607 peer-reviewed publications and 245,770 citations in last 5 years
- 1,004 postgraduate trainees (740 in 2013): 250 in Internal Medicine (PGY1–4), 142 in our PGY1 entry programs, 152 PGY4–PGY6 subspecialty trainees, and 460 fellows (441 clinical and 19 research)
The external review is a wonderful opportunity to take stock of where we are, and where we’d like to be, and to garner input on how to get there. Over the last five years, the Department has been focused on reassessment and renewal with a spotlight on enhancing diversity, equity and professionalism; the added value of the Department to its faculty and hospitals; divisional support, particularly for residency training; cross-departmental communication and branding; and transparency of our processes and decision-making.
Through improved branding, celebration and engagement (such as the redeveloped Department of Medicine postgraduate graduation ceremony and creation of an Associate Professors’ Day, just to name a few), we are working to develop a sense of “pride of place” and belonging in the University of Toronto and the Department of Medicine.

Our policies and procedures with respect to allocation of salary support, recruitment, senior promotion and leadership appointments, have been reviewed and revised as needed to increase fairness and transparency. This has improved faculty engagement in departmental efforts, including the merit review of clinician scientists and the formal search process for all new recruits and leadership roles.
Through the creation of a new Mentorship, Equity and Diversity leadership portfolio under Dr. Sharon Straus, we are addressing identified lack of equity and diversity among our trainees and faculty members, which requires attention also to professionalism.
Until recently, there has been a reluctance to discipline faculty members whose behaviour is uncivil or disrespectful or downright unprofessional, especially those who have gained acclaim for their academic contributions (we have called these the “untouchables”). This reluctance to discipline has had a negative impact on the culture within the Department and hospitals, affecting career satisfaction and wellness and the learner environment.
Outstanding efforts have been made by our leaders to address these issues – to work together to promote collegial culture, equity, diversity, inclusiveness and professionalism. It is not just talk, but action; a tangible shift in culture is occurring with demonstrable impact on the trainee/work environment and faculty career satisfaction. Professionalism is now baked into recruitment, renewal, award allocation, leadership appointment and senior promotion. Other departments at the University of Toronto and elsewhere are following our lead.
In 2015, the expectations of DDDs were revised and agreed upon, and leadership terms clarified. Ten external divisional reviews have been completed with a number planned for the upcoming academic year. A new division, Palliative Medicine, has been established to support a new Royal College residency training program in this discipline. Hospital vice presidents of research are now active participants in departmental reviews and recruitment and retention of our clinician scientist faculty.
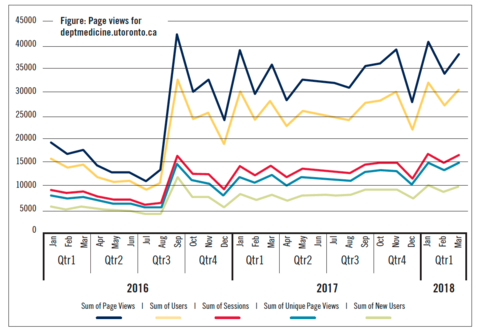
We’ve appointed a DoM Lead for Communications enabling more effective communication via our new website, newsletters and social media. On average, we receive more than 30,000 website page views per month now than we did prior to the development of new site.
The growing reputation of the University of Toronto and the Toronto-Waterloo corridor for entrepreneurism, particularly in the fields of big data, artificial intelligence (AI) and biotechnologies, has led to an influx of talent; tremendous opportunities present themselves to our Department. We have formally partnered with the Department of Computer Science in the recruitment of a recent PhD graduate from MIT in AI, Dr. Marzyeh Ghassemi, who is split 51:49 between Computer Science and Medicine. Ghassemi was named among the top 35 under 35 in her graduating class at MIT, and we are very excited that she has joined us.
Overall, I think we are in a good place. From our faculty surveys, career satisfaction is high. The University of Toronto and Toronto itself provide an extremely rich environment in which to provide clinical care, teach and conduct scholarly work. We are surrounded by the best minds in computer science, engineering, global health, public health and the fundamental sciences and by a thriving ecosystem for entrepreneurship. The diversity of the population in which we live and work provides an unequalled opportunity to lead the way in advancing equity, diversity and inclusion in academic medicine. People are drawn to Toronto and to the University of Toronto, specifically, by its international reputation and growing visibility in the artificial intelligence and big data realms. Our Dean is an outstanding supporter of the Department, championing the culture shift and values that our Department holds.
It takes a village to keep us in good shape – thank you to our Vice Chairs, PICs, Departmental Division Directors, Residency and Fellowship Program Directors, staff, trainees and all the many, many members of our faculty who help to keep things moving forward. Please have a look at our Vice Chairs’ summaries, included in this edition of DoM Matters.
On the whole, I am extremely pleased with the current status of the Department. We have a truly outstanding leadership team, and it is an honour to serve such an exceptional group of physicians, scientists, educators, innovators, staff and trainees. Given our size and strengths, we recognize that we can play a pivotal role in shaping policy and setting direction, not only for ourselves but also more broadly in the Faculty of Medicine. We are fortunate that the learners and faculty that we attract are inherently highly motivated to be the best they can be and to contribute meaningfully to patient care. As a result, I believe the most important role of the Chair and the leadership team is to break down barriers to the success of these individuals—to serve as catalysts, champions and facilitators. I believe that our collective work over the past five years to address unprofessionalism and inequities/lack of diversity in the workplace is doing just this. We will continue to break down the silos and biases that prevent us from being the best we can be. Increased attention to individual faculty wellness will further this goal.
Medical Education: Dr. Arno Kumagai
The past five years have witnessed great changes in medical education—both in the Department and Faculty of Medicine. Following the appointment of Dr. Arno Kumagai as the new Vice Chair for Education in 2016, the Department recruited a dynamic educational leadership team. Dr. Luke Devine was brought on as the Undergraduate Medical Medication lead, Dr. Jeannette Goguen as new Core Internal Medicine Residency Program Director and Director of PGY1 Programs, Dr. Eric Yu as Director for Subspecialty Programs, and Dr. Cheryl Jaigobin as Fellowship Director. This team has played a central role in facilitating major changes in the educational environment of the DoM, including the introduction of a new Foundations Curriculum and third-year Clerkship Renewal in the undergraduate MD Program; the staged nationwide implementation of Competence by Design (CBD) in all postgraduate training programs; and a top-to-bottom review and enhancement of all DoM fellowship programs. CBD in particular, is a challenging, resource-intensive initiative, and we have had the great fortune to have Dr. Scott Berry serving as the Faculty Lead of planning and implementation of CBD.
Several major new initiatives with in the DoM have been launched. An educational initiative in Person-Centred Care that includes teaching on equity, humanism, and social justice has been developed under the leadership of Drs. Lisa Richardson and Ayelet Kuper. The PCC initiative has involved curricular innovations from first-year medical students to subspecialty residents and has engaged faculty in developing skills for education through dialogue in clinical environments.
In collaboration with faculty members in the Division of General Internal Medicine, DoM Faculty Ambulatory Lead, Dr. Jakov Moric, has been coordinating the development of postgraduate Ambulatory Care Education through enhancement of existing ambulatory rotations and the planning and piloting of new rotations in a variety of unique settings, such as real-time subspecialty consultations in Family Medicine and outpatient rotations in refugee health and addiction medicine.
In addition to these new efforts, well-established DoM educational programs have continued to thrive. The Faculty-Resident Co-Learning Curriculum in Quality Innovation, led by Dr. Brian Wong, has continued to garner national and international attention; the Master Teacher Program has welcomed the addition of a new Co-Director, Dr. Umberin Najeeb, who joins Dr. Danny Panisko in leading one of the most important advanced faculty development programs in the U of T system for teaching clinical teachers; and Drs. Shiphra Ginsburg and Ryan Brydges have continued to promote medical education scholarship through the creation of a new DoM Research Network in Competence-Based Medical Education.
But, some of the most important achievements of the education portfolio have not been programmatic but cultural: a renewed commitment to issues of transparency, equity, inclusion, and professionalism in the learning climate and departmental processes, as well as efforts to recognize and celebrate the joy of teaching and learning the art and science of medicine.
Research & Scholarship: Dr. Michael Farkouh
The Department of Medicine’s research spans the spectrum of biomedical investigation. Research in the DoM is conducted on the U of T campus in the Medical Sciences Building, at the research institutes of our fully affiliated hospitals and at the hospitals themselves. At present, there are 200 clinician scientists and approximately 185 clinician investigators in the DoM. In our most recent survey, the DoM held approximately $185,448,000 in funded research across our university-wide enterprise, with over 1,900 individual awards, including 20 Canada Research Chairs held between 2012 and 2017. The following outlines major accomplishments in Research over the past five years.
Implementation of DoM Research Networks
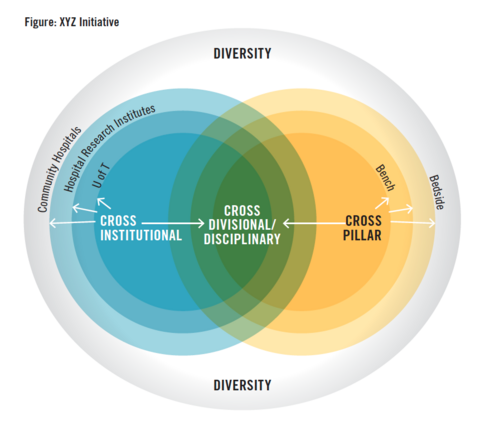
In 2016, the DoM decided to shift gears and use its resources to support novel network grant proposals to invigorate and promote collaboration not only across research institutes and pillars of research, but also across the health disciplines and divisions. This model was informed by the ground-breaking Toronto Dementia Research Alliance that was created under the visionary leadership of Dr. Sandra Black from the Division of Neurology. We term this the XYZ/D initiative (see figure below). With this model, we have been able to create nine collaborative research networks that are promoting cross-University multidisciplinary research and creating effective platforms to compete for federal funding.
Since 2015, we have created the following research networks:
- The Toronto Antimicrobial Resistance Research Network (TARRN)
- The General Medicine Inpatient Initiative (GEMINI)
- Critical Care Network
- Educational Research Network
- The HIV Network
- Infectious Global Health Threats
- Medical Oncology/Personalized Medicine
- Stroke Network
- Cardio/Rheumatology Network
The DoM Research Awards Committee
In 2016, the DoM’s Research Awards Committee was established to determine how to better recognize meritorious scientists with external awards. The committee is comprised of DoM scientists, many of whom have been recipients of international research awards, and Chairs of the DoM Promotions and Toronto Academic Health Sciences Network Research (TAHSN-R) Committees. This initiative has been well received and written up in a perspective by colleagues from St. Michael's Hospital entitled “Awards and Honours: Tricks of the Trade”. There have been several notable awards won by DoM faculty members. These include Frances Shepherd being awarded the 2018 Canada Gairdner Wightman Award.
Clinician Educator and Clinician Scientist (Phillipson Scholars) Training Programs
For the past 25 years, the Clinician Educator and Clinician Scientist Training Programs have been accepting clinician trainees to pursue graduate research training at the University of Toronto or select international universities. To date, these programs have trained over 100 individuals; approximately 70 per cent go on to assume academic research positions as clinician scientists or clinician educators. The calibre of the trainees selected to be part of the CSTP and CETP is demonstrated by the number of prestigious scholarships and grants awarded to them, including multiple CIHR fellowships and Vanier awards, during their time in the program.
Merit Review
In 2012, a merit review was established to vet applications for salary support to clinician scientists five years or more from their first faculty appointment. Researchers are eligible if they do not hold external salary support and are deemed meritorious in a competition directed by the Merit Review Committee, which is chaired by Dr. Kevin Kain. Since 2016, applications have mirrored the CIHR foundation scheme format.Awardees receive $40,000 per year for three years. In 2018, 12 awards were granted to scientists across nine divisions.
Industry Relations Committee
Because of perceived challenges in engaging with industry to support research, we have formed an Industry Relations Committee. This initiative aims to allow our scientists and investigators to evaluate new compounds and devices in accordance with University policy and engage increasingly in multicentre international clinical trials.
Quality and Innovation: Dr. Kaveh Shojania
So many faculty and trainees in the Department of Medicine now engage in quality improvement (QI) activities that it’s easy to forget how far we have come in the past five years. The DoM launched the Clinicians in Quality and Innovation (CQI) job description in 2012 with just four faculty—now there are more than 50. The Co-Learning Curriculum in Quality Improvement started with three subspecialty programs in Medicine, but has since spread to 35 training programs and over 200 residents, including not just Medicine, but also Paediatrics, Surgery, Anesthesia, and Laboratory Medicine & Pathobiology. We also now have many QI-specific initiatives and programs led by members of the Department, just a few of which are summarized below.
Women’s College Hospital Institute for Health System Solutions and Virtual Care (WIHV) leads the newly appointed Centre of Excellence (COE) in Digital Health Benefits Evaluation with nine core partners and over 20 supporting partners. Funded by the Ontario Ministry of Health and Long-Term Care (MOHLTC), this COE evaluates emerging tools and models of care for virtual care, telehealth, apps and wearables aimed at improved health. WIHV is also the preferred evaluator for demonstration projects conducted by the Ontario Telemedicine Network. Similarly, the National Research Council Industrial Research Assistance Program (NRC-IRAP) sought out WIHV to provide expertise to companies with digital health products. WIHV has contributed to or led the vetting of approximately 30 companies and their products in the digital health space.
General Medicine Inpatient Initiative (GEMINI), led by Drs. Fahad Razak and Amol Verma, is a collaboration focused on studying and improving care for general medicine patients in hospital, primarily using electronic clinical data. GEMINI has developed infrastructure to extract and standardize electronic clinical data from hospital IT systems (laboratory, radiology, pharmacy, etc.) at seven U of T-affiliated hospitals. It has quickly emerged as an exciting resource for translational research, with emerging projects with more than 30 researchers and 25 medical trainees. Attesting to this interest, MOHLTC and Health Quality Ontario has committed $4M to support the extension of GEMINI to include the 30 largest hospitals in Ontario over the next three years.
The Centre for Quality Improvement and Patient Safety (C-QuIPS) started with three core faculty (two from the DoM) in 2009. It now has 12 staff, 16 core members and more than 80 affiliated members, about $200,000 per year in revenue generated by its educational programs (with 1,188 graduates to date), $50M in grants obtained by core members, and 276 publications. External reviewers earlier this year described “the return on investment for CQuIPS as truly remarkable, and nothing short of spectacular.”
In addition to these three groups, Department members lead or play major roles in Choosing Wisely Canada, the Institute for Clinical and Evaluative Sciences (ICES), the Li Ka Shing Knowledge Institute, and OpenLab.
More recently, there have been two additional exciting developments involving the department’s activities in Quality and Innovation include:
- Appointing Dr. Andreas Laupacis to develop a strategy for Patient Involvement. The Department’s fundamental Guiding Principle is to “Ensure that the perspectives and experiences of our patients and their families drive our work.” The appointment of Dr. Laupacis reflects a commitment by Dr. Hawker and the Department to expand its leadership in this area.
- Partnering with Computer Science to recruit Dr. Marzyeh Ghassemi following her PhD from MIT and a post-doctoral fellowship at Google. Dr Ghassemi’s research focuses on harnessing machine learning algorithms to leverage healthcare data to make better clinical decisions and to predict things like the length of patient hospital stays or whether they will need interventions such as blood transfusions or ventilators. Locally, she will be doing this work through her Machine Learning for Health (ML4H) lab, and she has already started collaborating with clinical research and quality improvement-oriented faculty to test and refine her ideas.
The Department has systematically invested in supporting work in quality improvement and innovation. The DoM looks forward to continuing to lead in this area to enhance patient safety and healthcare quality.
Mentorship, Equity and Diversity: Dr. Sharon Straus
The Mentorship, Equity and Diversity (MED) portfolio was established in November 2015 to build on the Department’s commitment to faculty and trainee wellness and to develop policies and practices to increase fairness, equity and diversity. In particular, it was created in direct response to needs that faculty members identified via review of departmental data by gender, findings from the 2015 DoM faculty survey, and stakeholder interviews conducted by the Chair during the first few months of her first term.
The Chair heard your concerns and as such, created the MED portfolio. These processes identified a lack of sex and gender diversity in the Department, particularly among the higher academic ranks and leaders. Although 50 per cent or more of the graduating MD classes across Canada have been female for at least two decades, in 2014, only 36 per cent of DoM faculty members overall, and 25 per cent of full professors, were female. Stakeholder interviews also identified a general perception that the Department lacked fairness and transparency in its processes and procedures, including recruitment and promotion. The 2015 faculty survey identified that a substantial proportion of faculty respondents had either witnessed or personally experienced unprofessional behaviour in the workplace. Mentorship was felt to be inadequate; less than 50 per cent reported having a formal mentor.
To address these concerns, the Mentorship, Equity and Diversity Committee, currently co-chaired by Dr. Andrea Page and Dr. Caroline Chessex, undertook several initiatives including:
- a qualitative study to enhance understanding of the identified gender gap. It explored the perceptions and experiences of our faculty members and identified strategies to mitigate the gap;
- a qualitative study to explore the perceptions and experiences of our faculty members about professionalism and to devise strategies to address incivility;
- creating divisional mentorship facilitators and workshops to optimize mentorship and revamping the mentorship award;
- establishing the annual Summit for Women in Academic Medicine (WAM) to promote women in academic medicine;
- conducting the 2017 faculty survey to gather additional information about faculty concerns;
- creating and implementing Search Committee Guidelines to ensure that the search processes for the DoM are transparent and equitable;
- implementing assessments of professionalism within CFAR and Promotions, and
- attempting to promote an organizational culture shift that prioritizes equity, fairness and the collective instead of the individual.
These initiatives have led to increased access to and satisfaction with mentorship, noted on the 2017 Departmental survey; increased diversity amongst DoM leaders; and increased diversity amongst DoM faculty.
While we are proud of the many steps we have taken in a short time, we know there is still much work to be done to meet our faculty members’ needs. Moving forward, the MED Committee is looking to explore further faculty concerns, in particular, related to enhancing DoM diversity such as our underrepresentation of racialized and disabled physicians; promoting mentorship through career transitions; and promoting faculty wellness; all of which contribute to our ongoing work building a positive, transparent and equitable work environment with a strong, diverse leadership.
As always, we welcome your suggestions and contributions: please contact dom.events@utoronto.ca if you are interested in participating in MED initiatives or have suggestions of new initiatives that should be tackled.

